Evaluation of the Effectiveness of Lean Six Sigma Approach for SARS-CoV-2 RT-PCR Turnaround Time (TAT) Improvement at a Hospital-Based Tertiary Laboratory
DOI:
https://doi.org/10.21141/PJP.2023.03Keywords:
Lean six Sigma, SARS-CoV-2, turnaround timeAbstract
Objectives. This study aims to evaluate the effectiveness of the Lean Six Sigma approach in improving procedure for (TAT) of reverse transcriptase polymerase chain reaction (RT-PCR) for SARS-CoV-2 testing at The Medical City. Specific objectives of the study are to determine the following: 1) baseline sigma and average TAT (in hours); 2) post-implementation sigma and average TAT (in hours) 3) compare if there is a significant improvement between baseline and post-implementation sigma and average TAT (in hours) 4) effect on workflow efficiency.
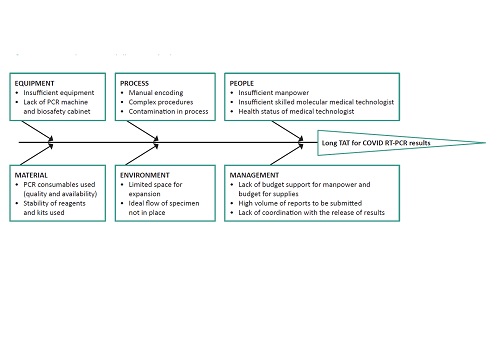
Methodology. Lean Six Sigma method for quality improvement was applied using DMAIC: Define, Measure, Improve, and Control. The root causes identified were lack of manpower, equipment, space, and manual and complex processes. Then, process wastes were identified, and corresponding proposed solutions were sustained in the control phase, such as standardization and the use of automation. Measurement of turn-around time and six sigma of the process were performed for evaluation.
Results. Results showed a significant improvement in the TAT in RT-PCR results, with most results released within 24 hours. The pre-Lean Six Sigma data on TAT were as follows: 24.88% released within 24 hours; 65.14% released within 24-48 hours; 3.56% released within 48-72 hours, and 6.42% released in more than 72 hours. The post Lean Six Sigma TAT were as follows: 95.32% released within 24 hours; 4.29% released within 24 to 48 hours; 0.13% released within 48-72 hours, and 0.12% released more than 72 hours. The computed sigma post-implementation was increased from 3.56 to 4.82. The p-value was calculated using the chi-square test, and the computed chi-square statistic is 1894.1021. The p-value is <0.00001 and the result is significant at p<.05. Although there is a significant decrease in the volume of samples post implementation due to the changing COVID19 situation, real time TAT was improved. It also resulted to increased workflow efficiency with the use of lesser manpower with more appropriate utilization.
Conclusion. Applying the Lean Six Sigma method to improve quality processes in the laboratory is shown to be practical, cost-effective, and straightforward.
Downloads
References
Villa D. Automation, lean, six sigma: synergies for improving laboratory efficiency. J Med Biochem. 2010:29:339-84 DOI: https://doi.org/10.2478/v10011-010-0038-3
Apostu SA, Vasile V, Veres C. Externalities of lean implementation in medical laboratories. process optimization vs. adaptation and flexibility for the future. Int J Environ Res Public Health. 2021;18(23):12309. https://pubmed.ncbi.nlm.nih.gov/34886029. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8657048. https://doi.org/10.3390/ijerph182312309. DOI: https://doi.org/10.3390/ijerph182312309
Inal TC, Goruroglu Ozturk O, Kibar F, et al. Lean six sigma methodologies improve clinical laboratory efficiency and reduce turnaround times. J Clin Lab Anal. 2018;32(1): e22180. https://pubmed.ncbi.nlm.nih.gov/28205271. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6817099. https://doi.org/10.1002/jcla.22180. DOI: https://doi.org/10.1002/jcla.22180
Sawalakhe PV, Deshmukh SV, Lakhe RR. Evaluating performance of testing laboratory using six sigma. Int J Innov Eng Sci. 2016;1(1):13-20.
Persis DJ, Anjali S, Vijaya Sunder M, Rejikumar G, Raja Sreedharan V, Saikouk, T. Improving patient care at a multi-speciality hospital using lean six sigma. Prod Plan Control. 2022;33(12):1135-54. DOI: https://doi.org/10.1080/09537287.2020.1852623
Letelier P, Guzmán N, Medina, G, et al. Workflow optimization in a clinical laboratory using lean management principles in the pre-analytical phase. J Med Biochem. 2020;40(1):26–32. https://pubmed.ncbi.nlm.nih.gov/33584137. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7857853. https://doi.org/10.5937/jomb0-26055. DOI: https://doi.org/10.5937/jomb0-26055
Morón-Castañeda LH, Useche-Bernal A, Morales-Reyes OL, et al. Impact of lean methodology to improve care processes and levels of satisfaction in patient’s care in a clinical laboratory. Rev Calid Asist. 2015;30(6):289–96.https://pubmed.ncbi.nlm.nih.gov/26546169. https://doi.org/10.1016/j.cali.2015.09.001. DOI: https://doi.org/10.1016/j.cali.2015.09.001
Kovach JV, Ingle D. Using lean six sigma to reduce patient cycle time in a nonprofit community clinic. Qual Manag Health Care. 2019;28(3):169–75. https://pubmed.ncbi.nlm.nih.gov/31246780. https://doi.org/10.1097/QMH.0000000000000215. DOI: https://doi.org/10.1097/QMH.0000000000000215
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 PJP

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.








