Coagulation and Platelet Profiles of COVID-19 Patients admitted to a COVID Referral Center from March 2020 to December 2022
DOI:
https://doi.org/10.21141/PJP2024.02Keywords:
coagulation, platelet test, activated partia thromboplastin time, APTT, COVID-19, disease severityAbstract
Objective. This study aimed to determine the demographic profiles of admitted COVID-19 patients, the association of coagulation and platelet tests on COVID-19 severity and compare the coagulation and platelet profile across the spectrum of the disease in terms of severity among adult COVID-19 patients admitted to the Philippine General Hospital from March 2020 to December 2022.
Methodology. Medical records of a sample of adult COVID-19 patients admitted to the emergency room of the Philippine General Hospital from March 2020 to December 2022 were reviewed. The demographics, initial COVID-19 diagnosis and initial coagulation and platelet test results were gathered and tabulated. Comparison of the initial coagulation and initial platelet results were made per disease category.
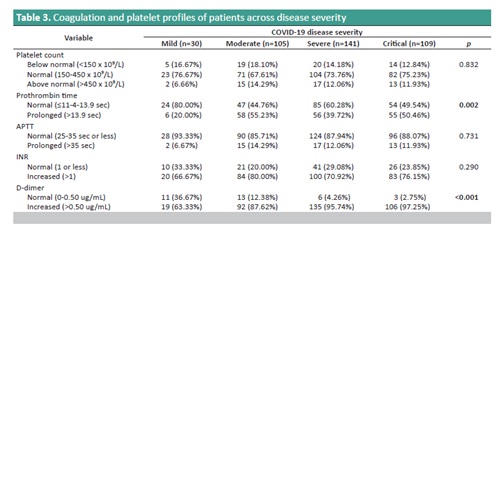
Results. Three hundred eighty-five (385) patients were included; 194 were males, and 191 were females. The mean age of all patients was 56.18 years old. There was a total of 30 patients classified as mild and 105 patients are under moderate category. 141 patients were classified as severe, whereas 109 patients were classified as critical. Platelet count test and Activated Partial Thromboplastin Time (APTT) were mostly normal in all disease categories. Prothrombin time was normal in a majority of patients from the mild and severe categories. INR and D-dimer were all elevated mostly in all disease categories.
Conclusion. Platelet counts and APTT were mostly normal in all disease categories. Prothrombin time and D-dimer had a significant association with disease severity. Platelet count, APTT and INR did not show significant association with disease severity. Prothrombin time, APTT, INR and D-dimer means had significant differences versus disease categories.
Downloads
References
WHO Coronavirus (COVID-19) Dashboard. (n.d.) June 22, 2023. https://data.who.int/dashboards/covid19/cases?n=c.
Department of Health COVID-19 Tracker. June 20, 2023. https://doh.gov.ph/diseases/covid-19/covid-19-case-tracker/.
WHO Chief declares end of COVID-19 as global health emergency. United Nations. May 5, 2023. https://news.un.org/en/story/2023/05/1136367.
Araya S, Mamo MA, Tsegay YG, et al. Blood coagulation parameter abnormalities in hospitalized patients with confirmed COVID-19 in Ethiopia. PloS One. 2021;16(6):e0252939. https://pubmed.ncbi.nlm.nih.gov/34153056. PMCID: PMC8216564. https://doi.org/10.1371/journal.pone.0252939. DOI: https://doi.org/10.1371/journal.pone.0252939
Umakanthan S, Sahu P, Ranade AV, et al. Origin, transmission, diagnosis and management of coronavirus disease 2019 (COVID-19). Postgrad Med J. 2020;96(1142):753-8. https://pubmed.ncbi.nlm.nih.gov/32563999. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10016932. https://doi.org/10.1136/postgradmedj-2020-138234.
Department of Health Circular No. 2002-0002. January 6, 2022. https://doh.gov.ph/sites/default/files/health-update/dc2022-0002.pdf.
Kaiafa GD, Savopoulos C, Karlafti E, et al. Coagulation profile of COVID-19 patients. Life (Basel). 2022;12(10):1658. https://pubmed.ncbi.nlm.nih.gov/36295093. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9604860. https://doi.org/10.3390/life12101658. DOI: https://doi.org/10.3390/life12101658
Abd El-Lateef AE, Alghamdi S, Ebid G, Khalil K, Kabrah S, Ghafar MTA. Coagulation profile in COVID-19 patients and its relation to disease severity and overall survival: a single-center study. Br J Biomed Sci. 2022:79:10098. https://pubmed.ncbi.nlm.nih.gov/35996516. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9302539. https://doi.org/10.3389/bjbs.2022.10098. DOI: https://doi.org/10.3389/bjbs.2022.10098
Wool GD, Miller JL. The impact of COVID-19 disease on platelets and coagulation. Pathobiology. 2021;88(1):15–27. https://pubmed.ncbi.nlm.nih.gov/33049751. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7649697. https://doi.org/10.1159/000512007. DOI: https://doi.org/10.1159/000512007
Corrêa TD, Cordioli RL, Campos Guerra JC, et al. Coagulation profile of COVID-19 patients admitted to the ICU: an exploratory study. PLoS One. 2020;15(12):e0243604. https://pubmed.ncbi.nlm.nih.gov/33320874. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7737963. https://doi.org/10.1371/journal.pone.0243604. DOI: https://doi.org/10.1371/journal.pone.0243604
Liao D, Zhou F, Luo L, et al. Haematological characteristics and risk factors in the classification and prognosis evaluation of COVID-19: a retrospective cohort study. Lancet Haematol. 2020;7(9):e671-8. https://pubmed.ncbi.nlm.nih.gov/32659214. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7351397. https://doi.org/10.1016/S2352-3026(20)30217-9. DOI: https://doi.org/10.1016/S2352-3026(20)30217-9
National Ethical Guidelines for Health and Health-Related Research 2017. https://ethics.healthresearch.ph/index.php/phoca-downloads/category/4-neg.
Feng Y, Ling Y, Bai T, et al. COVID-19 with different severities: a multicenter study of clinical features. Am J Respir Crit Care Med. 2020;201(11):1380-8. https://pubmed.ncbi.nlm.nih.gov/32275452. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7258639. https://doi.org/10.1164/rccm.202002-0445OC. DOI: https://doi.org/10.1164/rccm.202002-0445OC
Ibrahim ME, Al-Aklobi OS, Abomughaid MM, Al-Ghamdi MA. Epidemiological, clinical, and laboratory findings for patients of different age groups with confirmed coronavirus disease 2019 (COVID-19) in a hospital in Saudi Arabia. PLoS One. 2021;16(4):e0250955. https://pubmed.ncbi.nlm.nih.gov/33914805. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8084156. https://doi.org/10.1371/journal.pone.0250955. DOI: https://doi.org/10.1371/journal.pone.0250955
Shi Y, Yu X, Zhao H, Wang H, Zhao R, Sheng J. Host susceptibility to severe COVID-19 and establishment of a host risk score: findings of 487 cases outside Wuhan. Crit Care. 2020;24(1):108. https://pubmed.ncbi.nlm.nih.gov/32188484. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7081524. https://doi.org/10.1186/s13054-020-2833-7. DOI: https://doi.org/10.1186/s13054-020-2833-7
Lippi G, Plebani M, Henry BM. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta. 2020;506:145-8. https://pubmed.ncbi.nlm.nih.gov/32178975. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7102663. https://doi.org/10.1016/j.cca.2020.03.022. DOI: https://doi.org/10.1016/j.cca.2020.03.022
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 PJP

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.








