Baseline Complete Blood Count and Cell Population Data as Prognostic Markers for In-Hospital Mortality among COVID-19 Patients admitted at the Philippine General Hospital from March 2020 to January 2022
DOI:
https://doi.org/10.21141/PJP.2023.04Keywords:
COVID-19, hematology, blood cell count, complete blood count, prognosis, cell population dataAbstract
Introduction. Complete blood count (CBC) and cell population data (CPD) are hematologic parameters used in several clinical scenarios including infection and neoplastic processes. In the setting of COVID-19 infection, there is relative paucity of data in their use as possible prognostic markers.
Objective. We aim to evaluate the utility of the baseline CBC and CPD as prognostic markers for in-hospital mortality among COVID-19 patients admitted in Philippine General Hospital from March 2020 to January 2022.
Methodology. This is a case-control study. Expired patients served as cases, and recovered patients served as controls. Data from eligible patients including age, sex, admitting COVID diagnosis with severity, final disposition, baseline CBC and CPD results were collected from the hospital medical records and hematology section of the Department of Laboratories. Statistical analyses were done to determine the prognostic value of these parameters for in-hospital mortality.
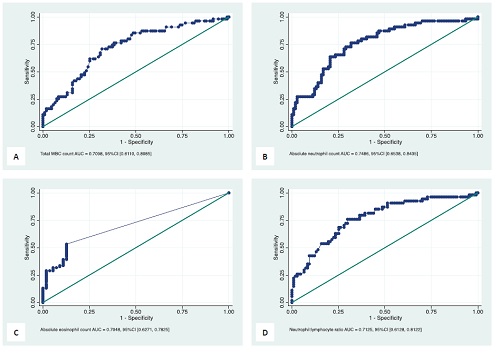
Results. Among the different CBC and CPD parameters, the study shows total white blood cell (WBC) count, absolute neutrophil count (ANC), absolute eosinophil count (AEC), and neutrophil-lymphocyte ratio (NLR) were statistically significant predictors for in-hospital mortality. For total WBC count, at a cut off 9.9 x 109/L, the sensitivity and specificity is 70.9% and 66.2%, respectively. For ANC, at a cut off of 7.3 x 109/L, the specificity is 76.4% and the specificity is 68.2%. At a cut off of 7.62, the NLR shows a sensitivity of 76.4% and specificity of 70.1%. For AEC, at a cut off of 0.006 x 109/L, the sensitivity is 53.3% and the specificity is 87.3%. AEC predicts towards the direction of survival rather than to the direction of in-hospital mortality.
Conclusion. The total WBC count, ANC, and NLR were statistically significant predictors for in-hospital mortality, while AEC predicts towards the direction of survival. The sensitivities and specificities of the cut off for these parameters were less than ideal. Correlation with clinical and other laboratory parameters is still recommended. For future studies, the authors recommend monitoring CBC and CPD parameters at different time points during the patients’ hospital course.
Downloads
References
WHO Coronavirus (COVID-19) Dashboard. World Health Organization. January 2022. https://covid19.who.int.
Rahman A, Niloofa R, Jayarajah U, De Mel S, Abeysuriya V, Seneviratne SL. Hematological abnormalities in COVID-19: a narrative review. Am J Trop Med Hyg. 2021;104(4):1188–201. https://pubmed.ncbi.nlm.nih.gov/33606667. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8045618. https://doi.org/10.4269/ajtmh.20-1536. DOI: https://doi.org/10.4269/ajtmh.20-1536
Huang I, Pranata R. Lymphopenia in severe coronavirus disease-2019 (COVID-19): systematic review and meta-analysis. J Intensive Care. 2020;8:36. https://pubmed.ncbi.nlm.nih.gov/32483488. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7245646. https://doi.org/10.1186/s40560-020-00453-4. DOI: https://doi.org/10.1186/s40560-020-00453-4
Yang X, Yang Q, Wang Y, et al. Thrombocytopenia and its association with mortality in patients with COVID-19. J Thromb Haemost. 2020;18(6):1469-72. https://pubmed.ncbi.nlm.nih.gov/32302435. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9906135. https://doi.org/10.1111/jth.14848. DOI: https://doi.org/10.1111/jth.14848
Wan S, Xiang Y, Fang W, et al. Clinical features and treatment of COVID-19 patients in northeast Chongqing. J Med Virol. 2020;92(7):797-806. https://pubmed.ncbi.nlm.nih.gov/32198776. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7228368. https://doi.org/10.1002/jmv.25783. DOI: https://doi.org/10.1002/jmv.25783
Lippi G, Mattiuzzi C. Hemoglobin value may be decreased in patients with severe coronavirus disease 2019. Hematol Transfus Cell Ther. 2020;42(2):116-7. https://pubmed.ncbi.nlm.nih.gov/32284281. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7128154. https://doi.org/10.1016/j.htct.2020.03.001. DOI: https://doi.org/10.1016/j.htct.2020.03.001
Yan X, Li F, Wang X, et al. Neutrophil to lymphocyte ratio as prognostic and predictive factor in patients with coronavirus disease 2019: A retrospective cross-sectional study. J Med Virol. 2020;92(11):2573-81. https://pubmed.ncbi.nlm.nih.gov/32458459. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7283791. https://doi.org/10.1002/jmv.26061. DOI: https://doi.org/10.1002/jmv.26061
Yang H, Xu Y, Li Z, Yan L, Wang J, Liao P. The clinical implication of dynamic hematological parameters in COVID-19: a retrospective study in Chongqing, China. Int J Gen Med. 2021;14:4073-80. https://pubmed.ncbi.nlm.nih.gov/34354369. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8331199. https://doi.org/10.2147/IJGM.S321292. DOI: https://doi.org/10.2147/IJGM.S321292
Waris A, Din M, Khalid A, et al. Evaluation of hematological parameters as an indicator of disease severity in Covid-19 patients: Pakistan's experience. J Clin Lab Anal. 2021;35(6):e23809. https://pubmed.ncbi.nlm.nih.gov/34028884. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8183923. https://doi.org/10.1002/jcla.23809. DOI: https://doi.org/10.1002/jcla.23809
Xu H, Zhong L, Deng J, et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020;12(1):8. https://pubmed.ncbi.nlm.nih.gov/32094336. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7039956. https://doi.org/10.1038/s41368-020-0074-x. DOI: https://doi.org/10.1038/s41368-020-0074-x
Tan L, Wang Q, Zhang D, et al. Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study. Signal Transduct Target Ther. 2020;5(1):33. https://pubmed.ncbi.nlm.nih.gov/32296069. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7100419. https://doi.org/10.1038/s41392-020-0148-4. DOI: https://doi.org/10.1038/s41392-020-0148-4
Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506. https://pubmed.ncbi.nlm.nih.gov/31986264. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7159299. https://doi.org/10.1016/S0140-6736(20)30183-5. DOI: https://doi.org/10.1016/S0140-6736(20)30183-5
Xu P, Zhou Q, Xu J. Mechanism of thrombocytopenia in COVID-19 patients. Ann Hematol. 2020;99(6):1205-8. https://pubmed.ncbi.nlm.nih.gov/32296910. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7156897. https://doi.org/10.1007/s00277-020-04019-0. DOI: https://doi.org/10.1007/s00277-020-04019-0
Urrechaga E. Reviewing the value of leukocytes cell population data (CPD) in the management of sepsis. Ann Transl Med. 2020;8(15):953. https://pubmed.ncbi.nlm.nih.gov/32953753. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7475430. https://doi.org/10.21037/atm-19-3173. DOI: https://doi.org/10.21037/atm-19-3173
Bhattacharya R, Koulmane Laxminarayana SL. Novel cell population data in Unicel DXH800 in the diagnosis of early sepsis. Int J Infect Dis. 2020;101(Suppl 1):182. https://doi.org/10.1016/j.ijid.2020.09.486. DOI: https://doi.org/10.1016/j.ijid.2020.09.486
Jung YJ, Kim JH, Park YJ, et al. Evaluation of cell population data on the UniCel DxH 800 Coulter Cellular Analysis system as a screening for viral infection in children. Int J Lab Hematol. 2012;34(3):283-9. https://pubmed.ncbi.nlm.nih.gov/22226427. https://doi.org/10.1111/j.1751-553X.2011.01392.x. DOI: https://doi.org/10.1111/j.1751-553X.2011.01392.x
Vasse M, Ballester MC, Ayaka D, et al. Interest of the cellular population data analysis as an aid in the early diagnosis of SARS-CoV-2 infection. Int J Lab Hematol. 2021;43(1):116-22. https://pubmed.ncbi.nlm.nih.gov/32812365. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7461522. https://doi.org/10.1111/ijlh.13312. DOI: https://doi.org/10.1111/ijlh.13312
Zeng X, Xing H, Wei Y, et al. Monocyte volumetric parameters and lymph index are increased in SARS-CoV-2 infection. Int J Lab Hematol. 2020;42(6):e266-9. https://pubmed.ncbi.nlm.nih.gov/32981233. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7537016. https://doi.org/10.1111/ijlh.13323. DOI: https://doi.org/10.1111/ijlh.13323
Palladino M. Complete blood count alterations in COVID-19 patients: a narrative review. Biochem Med (Zagreb). 2021;21(3):030501. https://pubmed.ncbi.nlm.nih.gov/34658642. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8495616. https://doi.org/10.11613/BM.2021.030501. DOI: https://doi.org/10.11613/BM.2021.030501
Pozdnyakova O, Connell NT, Battinelli EM, Connors JM, Fell G, Kim AS. Clinical significance of CBC and WBC morphology in the diagnosis and clinical course of COVID-19 infection. Am J Clin Pathol. 2021;155(3):364-75. https://pubmed.ncbi.nlm.nih.gov/33269374. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7799218. https://doi.org/10.1093/ajcp/aqaa231. DOI: https://doi.org/10.1093/ajcp/aqaa231
Lapić I, Brenčić T, Rogić D, et al. Cell population data: could a routine hematology analyzer aid in the differential diagnosis of COVID-19? Int J Lab Hematol. 2021;43(2):e64-7. https://pubmed.ncbi.nlm.nih.gov/33079479. https://doi.org/10.1111/ijlh.13368. DOI: https://doi.org/10.1111/ijlh.13368
Naoum FA, Ruiz A, Martin F, Brito T, Hassem V, Oliveira M. Diagnostic and prognostic utility of WBC counts and cell population data in patients with COVID-19. Int J Lab Hematol. 2021;43 Suppl 1 (Suppl 1):124-8. https://pubmed.ncbi.nlm.nih.gov/33190400. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7753689. https://doi.org/10.1111/ijlh.13395. DOI: https://doi.org/10.1111/ijlh.13395
Tan Y, Zhou J, Zhou Q, Hu L, Long Y. Role of eosinophils in the diagnosis and prognostic evaluation of COVID-19. J Med Virol. 2021;93(2):1105-19. https://pubmed.ncbi.nlm.nih.gov/32915476. https://doi.org/10.1002/jmv.26506. DOI: https://doi.org/10.1002/jmv.26506
Graña C, Ghosn L, Evrenoglou T, et al. Efficacy and safety of COVID-19 vaccines. Cochrane Database Syst Rev. 2022;2022(12):CD015477. https://doi.org/10.1002/14651858.CD015477. DOI: https://doi.org/10.1002/14651858.CD015477
Moghadas SM, Vilches TN, Zhang K, et al. The impact of vaccination on COVID-19 outbreaks in the United States. medRxiv. https://pubmed.ncbi.nlm.nih.gov/33269359. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7709178. https://doi.org/10.1101/2020.11.27.20240051. Preprint. DOI: https://doi.org/10.1101/2020.11.27.20240051
Lee CK, Merriam LT, Pearson JC, Lipnick MS, McKleroy W, Kim EY. Treating COVID-19: evolving approaches to evidence in a pandemic. Cell Rep Med. 2022;3(3):10053. https://pubmed.ncbi.nlm.nih.gov/35474746. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8826498. https://doi.org/10.1016/j.xcrm.2022.100533. DOI: https://doi.org/10.1016/j.xcrm.2022.100533
Khalid A, Ali Jaffar M, Khan T. et al. Hematological and biochemical parameters as diagnostic and prognostic markers in SARS-COV-2 infected patients of Pakistan: a retrospective comparative analysis. Hematology. 2021;26(1):529-42. https://pubmed.ncbi.nlm.nih.gov/34334100. https://doi.org/10.1080/16078454.2021.1950898. DOI: https://doi.org/10.1080/16078454.2021.1950898
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 PJP

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.








