Prevalence and Clinico-Pathologic Features of ALK Rearrangement Among Adult Filipinos with Non-Small Cell Lung Cancer in a Private Tertiary Care Hospital
DOI:
https://doi.org/10.21141/PJP.2022.04Keywords:
lung neoplasms, carcinoma non-small cell lung, anaplastic lymphoma kinase, flourescence in situ hybridizationAbstract
Introduction. With advancements in the understanding of lung cancer biology, targeted therapy has become the rule rather than the exception. Patients with ALK rearrangements are amenable to therapy with Alectinib and other ALK inhibitors, which has been associated with better patient outcomes. While ALK rearrangement should be routinely tested in non-squamous non-small cell lung cancer (NSCLC), the cost and availability of this test is a prohibitive factor, particularly in the Philippine setting.
Objectives. This study aimed (1) to determine the prevalence of ALK-rearranged NSCLC among adult Filipino lung cancer patients in St. Luke’s Medical Center (SLMC) from 2016 to 2018 and (2) to determine the clinico-pathologic features of adult Filipinos with ALK-rearranged NSCLC.
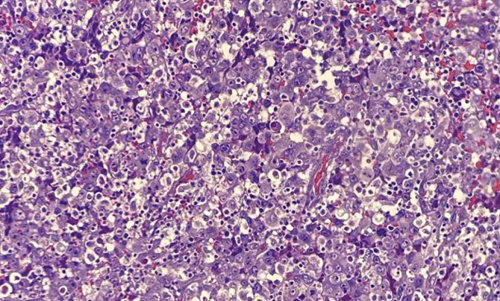
Methodology. This is a retrospective cross-sectional descriptive study wherein the prevalence of ALK-rearranged NSCLC, detected using fluorescence in-situ hybridization (FISH) or immunohistochemistry (IHC), was determined. Clinical data of patients for whom ALK testing was performed were collected. Hematoxylin and Eosin (H&E) slides were retrieved and reviewed for the presence of certain morphologic features. Patients whose H&E slides cannot be retrieved were excluded from the study.
Results. ALK rearrangement was seen in 7.8% (8/103) of tumors submitted for ALK testing. Patients with ALK-rearranged tumors were generally young, light smokers, and presented with advanced clinical stage. Clear cell features and solid pattern were noted in one case and three cases, respectively. However, due to small sample size, further statistical analysis could not be performed to analyze the association of these features with the presence of ALK rearrangement.
Conclusion. Despite a small sample size, the prevalence and clinical profile of ALK-rearranged NSCLC in our institution are congruent with those previously described in Western populations. The association of clinical profile and morphologic features with the presence of ALK rearrangement can be further explored in future studies.
Downloads
References
2. Ou SI, Zhu VW, Nagasaka M. Catalog of 5' fusion partners in ALK-positive NSCLC Circa 2020. JTO Clin Res Rep. 2020;1(1):100015. https://pubmed.ncbi.nlm.nih.gov/34589917. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8474466. https://doi.org/10.1016/j.jtocrr.2020.100015.
3. Rodig SJ, Mino-Kenudson M, Dacic S, et al. Unique clinicopathologic features characterize ALK-rearranged lung adenocarcinoma in the western population. Clin Cancer Res. 2009;15(16):5216-23. https://pubmed.ncbi.nlm.nih.gov/19671850. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2865649. https://doi.org/10.1158/1078-0432.CCR-09-0802.
4. Nishino M, Klepeis VE, Yeap BY, et al. Histologic and cytomorphologic features of ALK-rearranged lung adenocarcinomas. Mod Pathol. 2012;25(11):1462-72. https://pubmed.ncbi.nlm.nih.gov/22743652. https://doi.org/10.1038/modpathol.2012.109.
5. Shaw AT, Yeap BY, Mino-Kenudson M, et al. Clinical features and outcome of patients with non-small-cell lung cancer who harbor EML4- ALK. J Clin Oncol. 2009;27(26):4247-53. https://pubmed.ncbi.nlm.nih.gov/19667264. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2744268. https://doi.org/10.1200/JCO.2009.22.6993.
6. Solomon B, Lovly CM. Anaplastic lymphoma kinase (alk) fusion oncogene positive non-small cell lung cancer. UpToDate. https://www.uptodate.com/contents/anaplastic-lymphoma-kinase-alk-fusion-oncogene-positive-non-small-cell-lung-cancer#H3811658068. Accessed August 29, 2021.
7. Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG, eds. Tumours of the lung, pleura, and thymus. In: WHO classification of tumours, 4th ed, vol. 7. Switzerland: World Health Organization; 2020.
8. Bubendorf L, Lantuejoul S, de Langen AJ, Thunnissen E. Nonsmall cell lung carcinoma: diagnostic difficulties in small biopsies and cytological specimens. Eur Respir Rev. 2017;26(144):170007. https://pubmed.ncbi.nlm.nih.gov/28659503. https://doi.org/10.1183/16000617.0007-2017.
9. Minca EC, Lanigan CP, Reynolds JP, et al. ALK Status Testing in Non-Small Cell Lung Carcinoma by FISH on ThinPrep Slides with Cytology Material. J Thorac Oncol. 2014;9(4):464-8. https://pubmed.ncbi.nlm.nih.gov/24736067. https://doi.org/10.1097/JTO.0000000000000104.
10. Oki M, Yatabe Y, Saka H, et al. Feasibility and accuracy of molecular testing in specimens obtained with small biopsy forceps: comparison with the results of surgical specimens. Respiration. 2015; 89(3): 235-42. https://pubmed.ncbi.nlm.nih.gov/25676841. https://doi.org/10.1159/000369860.
11. Uruga H, Mino-Kenudson M. ALK (D5F3) CDx: an immunohistochemistry assay to identify ALK-positive NSCLC patients. Pharmgenomics Pers Med. 2018;11:147-55. https://pubmed.ncbi.nlm.nih.gov/30271189. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6147206. https://doi.org/10.2147/PGPM.S156672.
12. Lindeman NI, Cagle PT, Aisner DL, et al. Updated molecular testing guideline for the selection of lung cancer patients for treatment with targeted tyrosine kinase inhibitors: guideline from the College of American Pathologists, the International Association for the Study of Lung Cancer, and the Association for Molecular Pathology J Thorac Oncol. 2018;13(3): 323-58. https://pubmed.ncbi.nlm.nih.gov/29396253. https://doi.org/10.1016/j.jtho.2017.12.001.
13. National Comprehensive Cancer Network. Non-small cell lung cancer version 7.2021. https://www.nccn.org/guidelines/recently-published-guidelines. Accessed November 28, 2021.