Mucosal Schwann Cell Hamartoma Mimicking a Colon Polyp
Pathologic Insights
DOI:
https://doi.org/10.21141/PJP.2024.11Keywords:
schwann cell, hamartoma, mucosa, polyp, colorectalAbstract
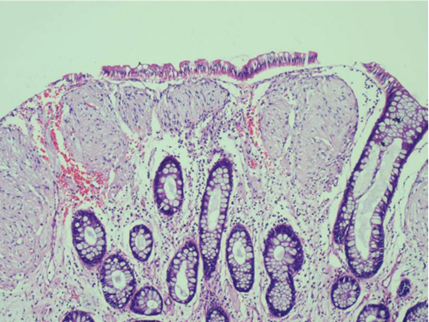
A rectal polyp is found during a routine colonoscopy of a 34-year-old male. He has no known significant family history of inherited disorder. Endoscopic findings reveal a 5-mm JNET 2A polyp in the rectum which is removed via forceps polypectomy. The microscopic examination shows a polypoid colonic mucosa with fairly circumscribed proliferation of low-grade spindle cells in the lamina propria, separating the crypts. The individual spindle cells are uniform in size with abundant eosinophilic cytoplasm. No mitotic figures, nuclear atypia, pleomorphism and necrosis are noted. Likewise, the crypts do not exhibit serrated architecture.
Downloads
References
Gibson JA, Hornick JL. Mucosal Schwann cell “hamartoma”: clinicopathologic study of 26 neural colorectal polyps distinct from neurofibromas and mucosal neuromas. Am J Surg Pathol. 2009;33(5):781–7. https://pubmed.ncbi.nlm.nih.gov/19065103 https://doi.org/10.1097/PAS.0b013e31818dd6ca DOI: https://doi.org/10.1097/PAS.0b013e31818dd6ca
Ismael F, Khawar S and Hamza A. Mucosal Schwann cell hamartoma of the gallbladder. Autops Case Rep. 2021;11:e2021338. https://pubmed.ncbi.nlm.nih.gov/34722355 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8552972 https://doi.org/10.4322/acr.2021.338 DOI: https://doi.org/10.4322/acr.2021.338
Feng X, Xu H, Dela Cruz N. Mucosal Schwann Cell Hamartoma in sigmoid colon – a rare case report and review of literature. Hum Pathol. 2020;19:200337. https://doi.org/10.1016/j.ehpc.2019.200337 DOI: https://doi.org/10.1016/j.ehpc.2019.200337
Han J, Chong Y, Tae-Jung K, et al. Mucosal Schwann cell hamartoma in colorectal mucosa: a rare benign lesion that resembles gastrointestinal neuroma. J Pathol Transl Med. 2017;51(2):187-9. https://pubmed.ncbi.nlm.nih.gov/27560153 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5357750 https://doi.org/10.4132/jptm.2016.07.02 DOI: https://doi.org/10.4132/jptm.2016.07.02
Goldblum JR, Lamps LW, McKenney JK, et al. Rosai and Ackerman's Surgical Pathology. Elsevier; 2018.
Beert E, Brems H, Renard M, et al. Biallelic inactivation of NF1 in a sporadic plexiform neurofibroma. Genes Chromosomes Cancer. 2012;51(9):852-7. https://pubmed.ncbi.nlm.nih.gov/22585738 https://doi.org/10.1002/gcc.21969 DOI: https://doi.org/10.1002/gcc.21969
Mann NS, Mann SK, Alam I. The safety of hot biopsy forceps in the removal of small colonic polyps. Digestion. 1999;60(1):74-6. https://pubmed.ncbi.nlm.nih.gov/9892802 https://doi.org/10.1159/000007592 DOI: https://doi.org/10.1159/000007592
Weiss SW, Goldblum JR. Enzinger and Weiss's Soft tissue tumors. Elsevier; 2020.
Lokuhetty D, White V, Watanabe R, Cree I, WHO classification of tumours editorial board. Digestive system tumours. 5th ed. Lyon: International Agency for Research on Cancer; 2019.
Groisman GM, Hershkovitz D, Vieth M, Sabo E. Colonic perineuriomas with and without crypt serration: a comparative study. Am J Surg Pathol. 2013;37(5):745-51. https://pubmed.ncbi.nlm.nih.gov/23588369 https://doi.org/10.1097/PAS.0b013e318277a1a9 DOI: https://doi.org/10.1097/PAS.0b013e318277a1a9
Hornick JL, Fletcher CD. Intestinal perineuriomas: clinicopathologic definition of a new anatomic subset in a series of 10 cases. Am J Surg Pathol. 2005;29(7):859-65. https://pubmed.ncbi.nlm.nih.gov/15958849 https://doi.org/10.1097/01.pas.0000154130.87219.2c DOI: https://doi.org/10.1097/01.pas.0000154130.87219.2c
Thway K, Fisher C. Diffuse ganglioneuromatosis in small intestine associated with neurofibromatosis type 1. Ann Diagn Pathol. 2009;13(1):50-4. https://pubmed.ncbi.nlm.nih.gov/19118783 https://doi.org/10.1016/j.anndiagpath.2007.06.001 DOI: https://doi.org/10.1016/j.anndiagpath.2007.06.001
Min KW, Leabu M. Interstitial cells of Cajal (ICC) and gastrointestinal stromal tumor (GIST): facts, speculations, and myths. J Cell Mol Med. 2006;10(4):995-1013. https://pubmed.ncbi.nlm.nih.gov/17125601 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3933091 https://doi.org/10.1111/j.1582-4934.2006.tb00541.x DOI: https://doi.org/10.1111/j.1582-4934.2006.tb00541.x
Rossi S, Miceli R, Messerini L, et al. Natural history of imatinib-naive GISTs: a retrospective analysis of 929 cases with long-term follow-up and development of a survival nomogram based on mitotic index and size as continuous variables. Am J Surg Pathol. 2011;35(11):1646-56. https://pubmed.ncbi.nlm.nih.gov/21997685 https://doi.org/10.1097/PAS.0b013e31822d63a7 DOI: https://doi.org/10.1097/PAS.0b013e31822d63a7
Miettinen M, Makhlouf H, Sobin LH, Lasota J. Gastrointestinal stromal tumors of the jejunum and ileum: a clinicopathologic, immunohistochemical, and molecular genetic study of 906 cases before imatinib with long-term follow-up. Am J Surg Pathol. 2006;30(4):477-89. https://pubmed.ncbi.nlm.nih.gov/16625094 https://doi.org/10.1097/00000478-200604000-00008 DOI: https://doi.org/10.1097/00000478-200604000-00008
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Marissa Krizelda Santos, Kathleen Adryon Tan

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.








