Mucosal Melanoma of the Male Urethra
A Case Report
DOI:
https://doi.org/10.21141/PJP.2023.14Keywords:
mucosal melanoma, urethra, genitourinary, urethral melanomaAbstract
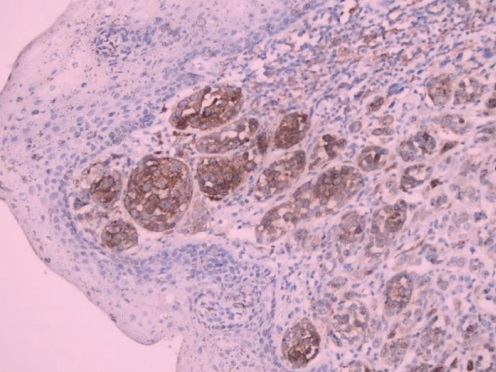
This is a rare case of a mucosal melanoma, located in the urethra of a 59-year-old male. Malignant melanomas of the genitourinary tract are rare, representing <1% of malignancies in the genitourinary tract, and <0.1% of all melanomas. In the male genitourinary tract, the most affected sites are the glans penis and the distal urethra in the fossa navicularis. Urethral melanomas comprise 4% of all urethral cancers.
Downloads
References
Scolyer RA. Melanocytic lesions. In: WHO Classification of Tumours Editorial Board. Urinary and male genital tumours. Lyon (France): International Agency for Research on Cancer; 2022 https://tumourclassification.iarc.who.int/chapters/36.
Bansal N, Garg G, Vashist S. Primary malignant melanoma of urethra mimicking as urethral caruncle. BMJ Case Rep. 2018;2018: bcr2018226056. https://pubmed.ncbi.nlm.nih.gov/30065058. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6069941. https://doi.org/10.1136/bcr-2018-226056. DOI: https://doi.org/10.1136/bcr-2018-226056
Altieri L, Wong MH, Peng D, Cockburn M. Mucosal melanomas in the racially diverse population of California. J Am Acad Dermatol. 2017;76(2):250-7. https://pubmed.ncbi.nlm.nih.gov/27742175. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7491918. https://doi.org/10.1016/j.jaad.2016.08.007. DOI: https://doi.org/10.1016/j.jaad.2016.08.007
Hansen MF, Abel I, Clasen-Linde E. Primary malignant melanoma of the urethra in a patient with rheumatoid arthritis treated with methotrexate. BMJ Case Rep. 2019;12(4):e228033. https://pubmed.ncbi.nlm.nih.gov/30948396. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6453280. https://doi.org/10.1136/bcr-2018-228033. DOI: https://doi.org/10.1136/bcr-2018-228033
Papeš D, Altarac S, Arslani N, Rajković Z, Antabak A, Ćaćić M. Melanoma of the glans penis and urethra. Urology. 2014;83(1):6–11. https://pubmed.ncbi.nlm.nih.gov/23978371. https://doi.org/10.1016/j.urology.2013.07.009. DOI: https://doi.org/10.1016/j.urology.2013.07.009
Jabiles AG, Del Mar EY, Pérez GAD, Vera FD, Montoya LMM, Deza CMM. Penile melanoma: a 20-year analysis of six patients at the National Cancer Institute of Peru, Lima. Ecacermedicalscience. 2017;11:731. https://pubmed.ncbi.nlm.nih.gov/28487750. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5406220. https://doi.org/10.3332/ecancer.2017.731. DOI: https://doi.org/10.3332/ecancer.2017.731
Safadi A, Schwalb S, Ben‐Shachar I, Katz R. Primary malignant urethral melanoma resembling a urethral caruncle. Urol Case Rep. 2017;15:28–9. https://pubmed.ncbi.nlm.nih.gov/28932693. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5596331. https://doi.org/10.1016/j.eucr.2017.08.004. DOI: https://doi.org/10.1016/j.eucr.2017.08.004
Aoki Y, Soma T, Nakamura Y, Fukui N, Sakai Y, Kageyama Y. Malignant melanoma of the male urethra with increased 5‐S‐cysteinyldopa: a case report. IJU Case Reports. 2019;2(4):215–7. https://pubmed.ncbi.nlm.nih.gov/32743417. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7292080. https://doi.org/10.1002/iju5.12086. DOI: https://doi.org/10.1002/iju5.12086
Rambhia PH, Scott JF, Vyas R, et al. Genitourinary melanoma. In: Scott JF, Gerstenblith MR, eds. Noncutaneous melanoma. Brisbane, Australia: Codon Publications; 2018. https://doi.org/10.15586/codon.noncutaneousmelanoma.2018.ch5. DOI: https://doi.org/10.15586/codon.noncutaneousmelanoma.2018.ch5
Murali R, Doubrovsky A, Watson GS, McKenzie PR, et al. Diagnosis of metastatic melanoma by fine-needle biopsy. Am J Clin Pathol. 2007;127(3):385–97. https://pubmed.ncbi.nlm.nih.gov/17276948. https://doi.org/10.1309/3QR4FC5PPWXA7N29. DOI: https://doi.org/10.1309/3QR4FC5PPWXA7N29
Omholt K, Grafström E, Kanter‐Lewensohn L, Hansson J, Ragnarsson-Olding B. KIT pathway alterations in mucosal melanomas of the vulva and other sites. Clin Cancer Res. 2011;17(12):3933–42. https://pubmed.ncbi.nlm.nih.gov/21680547. https://doi.org/10.1158/1078-0432.CCR-10-2917. DOI: https://doi.org/10.1158/1078-0432.CCR-10-2917
van Engen-van Grunsven ACH, Küsters-Vandevelde HVN, De Hullu J, et al. NRAS mutations are more prevalent than KIT mutations in melanoma of the female urogenital tract—a study of 24 cases from the Netherlands. Gynecol Oncol. 2014l;134(1):10–4. https://pubmed.ncbi.nlm.nih.gov/24802725. https://doi.org/10.1016/j.ygyno.2014.04.056. DOI: https://doi.org/10.1016/j.ygyno.2014.04.056
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 PJP

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.








