An Incidental Finding of Leydig Cell Tumor in a 36-year-old Southeast Asian Male who presents with Infertility
A Case Report and Literature Review
DOI:
https://doi.org/10.21141/PJP.2023.15Keywords:
Leydig cells, testis, orchiectomy, infertilityAbstract
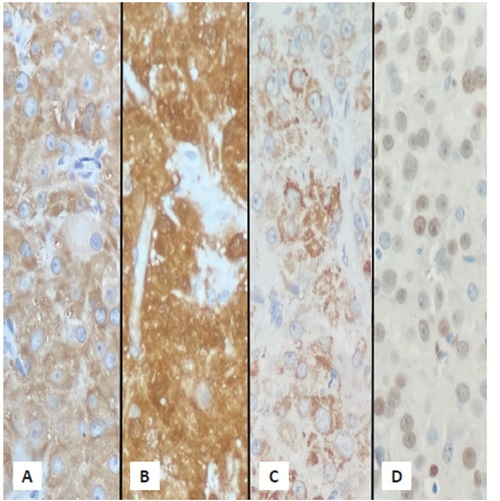
Leydig cell tumor is a rare testicular neoplasm that can present as a non-palpable small testicular nodule. Here we present a case of a 36-year-old Filipino male who initially came in for fertility work-up. Semen analysis showed azoospermia. However, an incidental finding on ultrasound showed a well-circumscribed round tumor. The patient underwent radical orchiectomy. On histopathologic examination, a Leydig cell tumor was identified and supported by immunohistochemical staining. We discuss the clinical features pathogenesis, treatment, diagnosis and prognosis of this uncommon entity.
Downloads
References
Zhou M, Netto GJ, Epstein JI. Uropathology. Elsevier; 2022.
Kim I, Young RH, Scully RE. Leydig cell tumors of the testis. A clinicopathological analysis of 40 cases and review of the literature. Am J Surg Pathol. 1985;9(3):177-92. https://pubmed.ncbi.nlm.nih.gov/3993830. https://doi.org/10.1097/00000478-198503000-00002. DOI: https://doi.org/10.1097/00000478-198503000-00002
Amin MB. WHO Classification of tumours: urinary and male genital tumours. International Agency for Research on Cancer; 2022.
Goldblum JR, Lamps LW, McKenney JK, Myers JL, Rosai J. Rosai and Ackerman’s Surgical Pathology. Elsevier; 2018.
Pomajzl AJ, Siref LE. Leydig cell cancer – Statpearls. 2023. Accessed April 2023. https://www.ncbi.nlm.nih.gov/books/NBK549800/.
Suardi N, Strada E, Colombo R, et al. Leydig cell tumour of the testis: presentation, therapy, long-term follow-up and the role of organ-sparing surgery in a single-institution experience. BJU Int. 2009;103(2):197-200. https://pubmed.ncbi.nlm.nih.gov/18990169. https://doi.org/10.1111/j.1464-410X.2008.08016.x. DOI: https://doi.org/10.1111/j.1464-410X.2008.08016.x
Hibi H, Yamashita K, Sumitomo M, Asada Y. Leydig cell tumor of the testis, presenting with azoospermia. Rep Med Biol. 2017;16(4):392-5. https://pubmed.ncbi.nlm.nih.gov/29259494. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5715892. https://doi.org/10.1002/rmb2.12046.
Kong Q, Yu Y, Tian T, Zhang H, Sun M, Liu R, Liu Y. Leydig cell tumor of a testis with azoospermia. Medicine (Baltimore). 2020;99(36):e22085. https://pubmed.ncbi.nlm.nih.gov/32899084. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7478542. https://doi.org/10.1097/MD.0000000000022085. DOI: https://doi.org/10.1097/MD.0000000000022085
Al-Agha OM, Axiotis CA. An in-depth look at Leydig cell tumor of the testis. Arch Pathol Lab Med. 2007;131(2):311-7. https://pubmed.ncbi.nlm.nih.gov/17284120. https://doi.org/10.5858/2007-131-311-AILALC. DOI: https://doi.org/10.5858/2007-131-311-AILALC
Fabiani A, Filosa A, Fioretti F, et al. Diagnostic ultrasound-guided excisional testicular biopsy for small (<1 cm) incidental nodules. A single institution experience. Arch Ital Urol Androl. 2014;86(4):373-7. https://pubmed.ncbi.nlm.nih.gov/25641474. https://doi.org/10.4081/aiua.2014.4.373. DOI: https://doi.org/10.4081/aiua.2014.4.373
Valentino M, Bertolotto M, Martino P, Barozzi L, Pavlica P. Incidentally detection of non-palpable testicular nodules at scrotal ultrasound: what is new? Arch Ital Urol Androl. 2014;86(4):378-82. https://pubmed.ncbi.nlm.nih.gov/25641475. https://doi.org/10.4081/aiua.2014.4.378. DOI: https://doi.org/10.4081/aiua.2014.4.378
Pozza C, Pofi R, Tenuta M, et al. Clinical presentation, management and follow-up of 83 patients with Leydig cell tumors of the testis: a prospective case-cohort study. Hum Rep. 2019;34(8):1389-403. https://pubmed.ncbi.nlm.nih.gov/31532522. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6688875. https://doi.org/10.1093/humrep/dez083. DOI: https://doi.org/10.1093/humrep/dez083
McCluggage WG, Shanks JH, Arthur K, Banerjee SS. Cellular proliferation and nuclear ploidy assessments augment established prognostic factors in predicting malignancy in testicular Leydig cell tumours. Histopathology. 1998;33(4):361-8. https://pubmed.ncbi.nlm.nih.gov/9822927. https://doi.org/10.1046/j.1365-2559.1998.00484.x. DOI: https://doi.org/10.1046/j.1365-2559.1998.00484.x
Ruf CG, Sanatgar N, Isbarn H, et al. Leydig-cell tumour of the testis: Retrospective analysis of clinical and therapeutic features in 204 cases. World J Urol. 2020;38(11):2857-62. https://pubmed.ncbi.nlm.nih.gov/31960106. https://doi.org/10.1007/s00345-020-03079-1.
Fankhauser CD, Grogg JB, Hayoz S, et al. Risk factors and treatment outcomes of 1,375 patients with testicular Leydig cell tumors: analysis of published case series data. J Urol. 2020;203(5):949-56. https://pubmed.ncbi.nlm.nih.gov/31845841. https://doi.org/10.1097/JU.0000000000000705. DOI: https://doi.org/10.1097/JU.0000000000000705
Weidemann S, Noori NA, Lennartz M, et al. Inhibin alpha expression in human tumors: A tissue microarray study on 12,212 tumors. Biomedicines. 2022;10(10):2507. https://pubmed.ncbi.nlm.nih.gov/36289769. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9598868. https://doi.org/10.3390/biomedicines10102507. DOI: https://doi.org/10.3390/biomedicines10102507
Busam KJ, Iversen K, Coplan KA, et al. Immunoreactivity for A103, an antibody to melan-A (Mart-1), in adrenocortical and other steroid tumors. Am J Surg Pathol. 1998;22(1):57-63. https://pubmed.ncbi.nlm.nih.gov/9422316. https://doi.org/10.1097/00000478-199801000-00007. DOI: https://doi.org/10.1097/00000478-199801000-00007
Sajjad Y, Quenby SM, Nickson P, Lewis-Jones DI, Vince G. Expression of androgen receptors in upper human fetal reproductive tract. Hum Rep. 2004;19(7):1659-65. https://pubmed.ncbi.nlm.nih.gov/15117891. https://doi.org/10.1093/humrep/deh295. DOI: https://doi.org/10.1093/humrep/deh295
Xu W, Zhu Q, Zhang B, et al. Protective effect of calretinin on testicular Leydig cells via the inhibition of apoptosis. Aging (Albany NY). 2017;9(4):1269-79. https://pubmed.ncbi.nlm.nih.gov/28437248. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5425126. https://doi.org/10.18632/aging.101226. DOI: https://doi.org/10.18632/aging.101226
Hibi H, Yamashita K, Sumitomo M, Asada Y. Leydig cell tumor of the testis, presenting with azoospermia. Rep Med Biol. 2017;16(4):392-5. https://pubmed.ncbi.nlm.nih.gov/29259494. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5715892. https://doi.org/10.1002/rmb2.12046. DOI: https://doi.org/10.1002/rmb2.12046
Giannarini G, Mogorovich A, Menchini Fabris F, et al. Long-term follow-up after elective testis sparing surgery for Leydig cell tumors: a single center experience. J Urol. 2007;178(3):872-6. https://pubmed.ncbi.nlm.nih.gov/7631320. https://doi.org/10.1016/j.juro.2007.05.077. DOI: https://doi.org/10.1016/j.juro.2007.05.077
Ruf CG, Sanatgar N, Isbarn H, et al. Leydig-cell tumour of the testis: Retrospective analysis of clinical and therapeutic features in 204 cases. World J Urol. 2020;38(11):2857-62. https://pubmed.ncbi.nlm.nih.gov/31960106. https://doi.org/10.1007/s00345-020-03079-1. DOI: https://doi.org/10.1007/s00345-020-03079-1
Leonhartsberger N, Pichler R, Stoehr B, Horninger W, Steiner H. Organ-sparing surgery is the treatment of choice in benign testicular tumors. World J Urol. 2013;32(4):1087-91. https://pubmed.ncbi.nlm.nih.gov/24092276. https://doi.org/10.1007/s00345-013-1174-4. DOI: https://doi.org/10.1007/s00345-013-1174-4
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 PJP

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.








