Impact of the COVID-19 Pandemic on Blood Supply
A Comparative Cross-Sectional Study of the Pre-Pandemic and Pandemic Era
DOI:
https://doi.org/10.21141/PJP.2023.11Keywords:
COVID-29 pandemic, blood donors, Philippines, fresh frozen plasma, whole blood, packed RBC, platelet concentrate, Davao CityAbstract
Objective. The study aimed to determine the impact of the COVID-19 pandemic on local blood supply management in the Davao Region, Philippines from 2019 to 2021 through the analysis of trends in blood supply in Davao Region, Philippines.
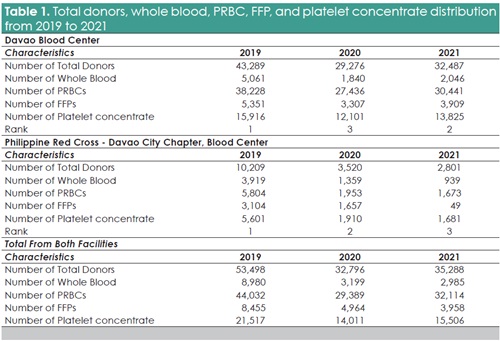
Methodology. Secondary data from two blood centers in the Davao Region for the years 2019 to 2021 were used to determine the trends on blood donation supply. To evaluate trends, the overall number of blood donors and the quantities of various types of blood components in whole blood, packed red blood cells (PRBCs), fresh frozen plasma (FFPs) and platelet concentrate have been compared between pre-pandemic, pandemic periods and as restrictions eased.
Results. A substantial decrease of 51.6% in the number of blood donors was seen during 2021 in comparison with 2019. The trend in collection by blood components also showed a significant trend from 2019 to 2021, whole blood (200.8%), packed RBCs (37.1%), fresh frozen plasma (113.6%). While the platelet concentrate supply declined by 34.9% from 2019 to 2020, an increase of 10.7% was noted onwards to 2021.
Conclusion. The results demonstrate that during the COVID-19 pandemic, there was a major reduction in donation and supply of blood. The challenges faced by blood banks in ensuring a stable and sufficient blood supply are highlighted by the decrease in the number of donors and by the different trends in the supply of blood components. The targeted efforts to promote blood donation and enhance the resilience of the blood supply during and after the pandemic is important.
Downloads
References
Okoroiwa HU, Okafor IM, Asemota EA, Ogar CO, Uchendu IK. Coping with COVID-19 pandemic in blood transfusion services in West Africa: the need to restrategize. Hematol Transfus Cell Ther. 2021;43(2):119-25. https://pubmed.ncbi.nlm.nih.gov/33714719. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8211632. https://doi.org/10.1016/j.htct.2021.01.005. DOI: https://doi.org/10.1016/j.htct.2021.01.005
Nicomedes CJC, Avila RMA. An analysis on the panic during COVID-19 pandemic through an online form. J Affect Disord. 2020;276:14-22. https://pubmed.ncbi.nlm.nih.gov/32697692. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7362858. https://doi.org/10.1016/j.jad.2020.06.046. DOI: https://doi.org/10.1016/j.jad.2020.06.046
Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020.;91(1):157-60. https://pubmed.ncbi.nlm.nih.gov/32191675. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7569573. https://doi.org/10.23750/abm.v91i1.9397.
Kumar S, Azim D, Nasim S, Hashmi SH. Dwindling blood reserves: an ominous downside of COVID-19 pandemic. Transfus Apher Sci. 202;59(5):102818. https://pubmed.ncbi.nlm.nih.gov/32487511. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7239777. https://doi.org/10.1016/j.transci.2020.102818. DOI: https://doi.org/10.1016/j.transci.2020.102818
Veseli B, Sandner S, Studte S, Clement M. The impact of COVID-19 on blood donations. PLoS ONE. 2022;17(3): e0265171. https://pubmed.ncbi.nlm.nih.gov/35324952. DOI: https://doi.org/10.1371/journal.pone.0265171
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC894667. https://doi. org/10.1371/journal.pone.0265171.
Shander A, Goobie SM, Warner MA, et al. Essential role of patient blood management in a pandemic: a call for action. Anesth Analg. 2020;131(1):74–85. https://pubmed.ncbi.nlm.nih.gov/32243296. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7173035. https://doi.org/10.1213/ANE.0000000000004844. DOI: https://doi.org/10.1213/ANE.0000000000004844
Chang L, Yan Y, Wang L. Coronavirus disease 2019: coronaviruses and blood safety. Transfusion medicine reviews. 2020;34(2):75–80. https://pubmed.ncbi.nlm.nih.gov/32107119. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7135848. https://doi.org/10.1016/j.tmrv.2020.02.003 DOI: https://doi.org/10.1016/j.tmrv.2020.02.003
Stanworth SJ, New HV, Apelseth TO, et al. Effects of the COVID-19 pandemic on supply and use of blood for transfusion. Lancet Haematol. 2020;7(10):e756–64. https://pubmed.ncbi.nlm.nih.gov/32628911. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7333996. https://doi.org/10.1016/S2352-3026(20)30186-1. DOI: https://doi.org/10.1016/S2352-3026(20)30186-1
Abdel Gader AG, Osman AM, Al Gahtani FH, Farghali MN, Ramadan AH, Al-Momen AK. Attitude to blood donation in Saudi Arabia. Asian J Transfus Sci. 2011;5(2):121–6. https://pubmed.ncbi.nlm.nih.gov/21897588. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3159239. https://doi.org10.4103/0973-6247.83235. DOI: https://doi.org/10.4103/0973-6247.83235
Gupta D. Voluntary blood donation: challenges in COVID-19 pandemic—Indian scenario. Ann Blood. 2020;5:21. https://doi.org/10.21037/aob-20-54. DOI: https://doi.org/10.21037/aob-20-54
Miskeen E, Yahia AIO, Eljack TB, Karar HK. The Impact of COVID-19 pandemic on blood transfusion services: a perspective from health professionals and donors. J Multidiscip Health. 2021;14:3063–71. https://pubmed.ncbi.nlm.nih.gov/34754194. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8572088. https://doi.org/10.2147/JMDH.S337039. DOI: https://doi.org/10.2147/JMDH.S337039
Raturi M, Kusum, A. The blood supply management amid the COVID-19 outbreak. Transfus Clin Biol. 2020;27)3):147-51. https://pubmed.ncbi.nlm.nih.gov/32386966. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7194633. https://doi.org/10.1016/j.tracli.2020.04.002. DOI: https://doi.org/10.1016/j.tracli.2020.04.002
Edrada EM, Lopez EB, Villarama JB, et al. Correction to: First COVID-19 infections in the Philippines: a case report. Trop Med Health. 2020;48:30. https://pubmed.ncbi.nlm.nih.gov/32390757. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7203260. https://doi.org/10.1186/s41182-020-00218-7. DOI: https://doi.org/10.1186/s41182-020-00218-7
Lumawag RJ. DOH confirms first Covid-19 case in Davao. Sun Star. Retrieved April 14,2020.
Davao City shifts to GCQ, few lockdown measures eased. City Government of Davao. May 15, 2020. https://www.davaocity.gov.ph/local-government/davao-city-shifts-to-gcq-few-lockdown-measures-eased/.
Chandler T, Neumann-Böhme S, Sabat I, et al. Blood donation in times of crisis: Early insight into the impact of COVID-19 on blood donors and their motivation to donate across European countries. Vox Sang. 2021;116(10):1031-41. https://pubmed.ncbi.nlm.nih.gov/33835509. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8250750. https://doi.org/10.1111/vox.13103. DOI: https://doi.org/10.1111/vox.13103
Mappala ACA, Alican CAL, Dulay DCT, Mancita SCA, Utanes BYG, Clemente BM. Factors affecting voluntary blood donations among adults in Metro Manila, Philippines, as a basis for policy improvement on donor recruitment. Acta Med Philipp. 2023;57(5):73-81. https://doi.org/10.47895/amp.vi0.4351. DOI: https://doi.org/10.47895/amp.vi0.4351
Loua A, Kasilo OMJ, Nikiema JB, Sougou AS, Kniazkov S, Annan, EA. Impact of the COVID‐19 pandemic on blood supply and demand in the WHO African region. Vox Sang. 2021;116(7):774-84. https://pubmed.ncbi.nlm.nih.gov/33529421. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8014179. https://doi.org/10.1111/vox.13071. DOI: https://doi.org/10.1111/vox.13071
Rafiee MH, Kafiabad SA, Maghsudlu M. Analysis of blood donors’ characteristics and deferrals related to COVID-19 in Iran. Transfus Apher Sci. 2021;60(2):103049. https://pubmed.ncbi.nlm.nih.gov/33468406. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7833597. https://doi.org/10.1016/j.transci.2020.103049. DOI: https://doi.org/10.1016/j.transci.2020.103049
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 PJP

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.

The Philippine Journal of Pathology is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. Based on works made open access at http://philippinejournalofpathology.org