Preliminary Study on Prevalence of P16-Positive Squamous Cell Carcinoma of the Oral Cavity, Oropharynx and Larynx in Rizal Medical Center and its Histomorphologic Correlation
DOI:
https://doi.org/10.21141/PJP.2022.08Keywords:
papillomavirus infections, squamous cell carcinoma of head and neck, mouth, larynxAbstract
Background. A considerably large portion of the cases of cancer, particularly squamous cell carcinoma (SCC) involving the head and the neck may be due to consumption of tobacco and alcohol. However, its increase in occurrence at specific sites of the head and neck may indicate the possibility of other etiological factors. One of which is infection by certain high-risk human papillomavirus (HPV). P16 immunochemistry serves as a very good surrogate marker of active HPV in these tumors. The detection of HPV-related head and neck cancers have relevance in clinical practice because of its prognostic implications.
Objectives. The general objective of this study is to determine the prevalence of p16-positive squamous cell carcinoma in the oral cavity, oropharynx, and larynx in Rizal Medical Center from January 2019 to December 2019. The specific objective is to compare the Hematoxylin and Eosin (H&E) stain histomorphology (keratinization and mitotic activity) of p16-positive versus p16-negative specimens.
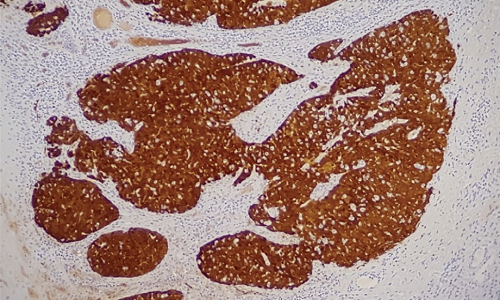
Methodology. This is a cross-sectional study which included all routine histopathology specimens coming from the oral cavity, oropharynx and larynx in Rizal Medical Center for the year 2019 with a diagnosis of squamous cell carcinoma. The tissue specimens considered were those that measured at least 1 cm in diameter, or aggregate diameter if tissue is fragmented. The slides of all eligible cases were reviewed and immunohistochemically stained for p16. The p16 IHC slides were read as either positive or negative, while the mitotic activity and keratinization were observed in the H&E-stained slides. The interpretation of the diplomate pathologists for each of the slides were documented and corresponding statistical analyses were performed.
Results. P16 IHC showed twenty-one (88%) p16 negative cases and three (12%) p16 positive cases. In terms of mitosis, ten cases have mitosis falling within the 1-10 per high power field (HPF) range (42%), six within 11-20 per HPF (25%), and 8 cases have ≥21 mitosis per HPF (33%). In terms of keratinization, three cases are non-keratinizing (12%) and twenty-one cases are keratinizing (88%). There is significant difference in the keratinization histology (p<0.05) of the p16-positive versus the P16-negative cases. On the other hand, no significant difference in the mitotic activity (p>0.05) was noted.
Conclusion. There is a low prevalence of HPV-related SCC of the oral cavity, oropharynx, and larynx in Rizal Medical Center. The histomorphologic findings confirm that keratinization, significantly predicts HPV status in oropharyngeal SCC. Mitotic activity may not be reliable in predicting the HPV status or p16 IHC reactivity of a case. Keratinization in oropharyngeal SCCs may provide valuable information in certain instances, particularly when HPV testing is not immediately available, although the combined tumor morphology and p16 IHC is more ideal.
Downloads
References
2. Van Dyne EA, Henly SJ, Saraiya M, Thomas CC, Markowitz LE, Bernard VB.Trends in human papillomavirus-associated cancers – United States, 1999-2015. MMWR Morb Mortal Wkly Rep. 2018;67(33):918-24. https://pubmed.ncbi.nlm.nih.gov/30138307. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6107321. https://doi.org/10.15585/mmwr.mm6733a2.
3. Albano P, Holzinger D, Salvador C, et al. Low prevalence of human papillomavirus in head and neck squamous cell carcinoma in the northwest region of the Philippines. PLoS ONE. 2017;12(2):e0172240. https://pubmed.ncbi.nlm.nih.gov/28199413. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5310881. https://doi.org/10.1371/journal.pone.0172240.
4. Cunningham L, Pagano G, Tandon R, et al. Overexpression of p16INK4 is a reliable marker of human papillomavirus-induced oral high grade squamous dysplasia. Oral Surg Oral Med Oral Pathol Oral radiol Endod. 2006;102(1):77-81. https://pubmed.ncbi.nlm.nih.gov/16831676. https://doi.org/10.1016/j.tripleo.2005.11.028.
5. Pfister D, Spencer S, Adelstein D, et al. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Head and Neck Cancers, version 1.2018-Feb. 15, 2018. Retrieved from oncolife.com.ua/doc/nccn/Head_and_Neck_Cancers.pdf.
6. Mehanna H, Paleri V, West CML, Nutting C. Head and neck cancer -- part 1: epidemiology, presentation, and prevention. BMJ. 2010;341:c4684. https://pubmed.ncbi.nlm.nih.gov/20855405. https://doi.org/10.1136/bmj.c4684.
7. Ferlay J, Soerjomataram I, Ervik M, et al. Dikshit R. GLOBOCAN 2012 v1.0, cancer incidence and mortality worldwide: IARC cancer base no. 11. International Agency for Research on Cancer, Lyon; 2014.
8. Sturgis EM, Ang KK. The epidemic of HPV-associated oropharyngeal cancer is here: is it time to change our treatment paradigms? J Natl Compr Canc Netw. 2011;9(6):665-73. https://pubmed.ncbi.nlm.nih.gov/21636538. https://doi.org/10.6004/jnccn.2011.0055.
9. Ang KK, Harris J, Wheeler R, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363(1):24-35. https://pubmed.ncbi.nlm.nih.gov/20530316. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2943767. https://doi.org/10.1056/NEJMoa0912217.
10. Ndiaye C, Mena M, Laia Alemany, et al. HPV DNA, E6/E7 mRNA and p16INK4a detection in head and neck cancers: a systemic review and meta-analysis. Lancet Oncol. 2014;15(12):1319-31. https://pubmed.ncbi.nlm.nih.gov/25439690. https://doi.org/10.1016/S1470-2045(14)70471-1.
11. Chaturvedi AK, Anderson WF, Lortet-Tieulent J, et al. Worldwide trends in incidence rates for oral cavity and oropharyngeal cancers. J Clin Oncol. 201;31(36):4550-9. https://pubmed.ncbi.nlm.nih.gov/24248688. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3865341. https://doi.org/10.1200/JCO.2013.50.3870.
12. Kjaer SK, Chackerian B, van den Brule AJ, et al. High-risk human papillomavirus is sexually transmitted: evidence from a follow-up study of virgins starting sexual activity (intercourse). Cancer Epidemiol Biomarkers Prev. 2001;10(2):101-6. https://pubmed.ncbi.nlm.nih.gov/11219765.
13. Marron M, Boffetta P, Zhang Z, et al, Cessation of alcohol drinking, tobacco smoking and the reversal of head and neck cancer risk. Int J Epidemiol. 2010;39(1):182-96. https://pubmed.ncbi.nlm.nih.gov/19805488. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2817090. https://doi.org/10.1093/ije/dyp291.
14. Duncan LD, Winkler M, Carlson ER, Heidel RE, Kang E, Webb D. p16 immunochemistry can be used to detect human papillomavirus in oral cavity squamous cell carcinoma. J Oral Maxillofac Surg. 2013;71(8):1367-75. MID: 23642549 https://doi.org/10.1016/j.joms.2013.02.019.
15. Lydiatt W, Patel SG, O’Sullivan B, et al, Head and neck cancers—major changes in the american joint committee on cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017;67(2):122-37. https://pubmed.ncbi.nlm.nih.gov/28128848. https://doi.org/10.3322/caac.21389.
16. Molony P, Werner R, Martin C, et al. The role of tumour morphology in assigning HPV status in oropharyngeal squamous cell carcinoma. Oral Oncology. 2020;105:104670. https://pubmed.ncbi.nlm.nih.gov/32279011. https://doi.org/10.1016/j.oraloncology.2020.104670.
17. Sedaghat AR, Zhang Z, Begum S et al. Prognostic significance of human papillomavirus in oropharyngeal squamous cell carcinomas. Laryngoscope. 2009;119(8):1542-9. https://pubmed.ncbi.nlm.nih.gov/19522004. https://doi.org/10.1002/lary.20533.
18. Marur S, Burtness B. Oropharyngeal squamous cell carcinoma treatment: current standards and future directions. Curr Opin Oncol. 2014;26(3):252-8. https://pubmed.ncbi.nlm.nih.gov/24626127. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5813288. https://doi.org/10.1097/CCO.0000000000000072.
19. Schlecht N, Masika M, Diaz A, et al. Risk of oral human papillomavirus infection among sexually active female adolescents receiving the quadrivalent vaccine. JAMA Netw Open. 2019;2(10): e1914031. https://pubmed.ncbi.nlm.nih.gov/31651968. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6822084. https://doi.org/10.1001/jamanetworkopen.2019.14031.
20. Nelson R. Gardasil-9 approved for prevention of head and neck cancers. Medscape Medical News. 2020. https://www.medscape.com/viewarticle/932369.
21. Chernock RD. Morphologic features of conventional squamous cell carcinoma of the oropharynx: ‘keratinizing’ and ‘nonkeratinizing’ histology types as the basis for a consistent classification system. Head and Neck Pathol. 2012;6 Suppl 1 (Suppl 1):S41-7. https://pubmed.ncbi.nlm.nih.gov/22782222. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3394167. https://doi.org/10.1007/s12105-012-0373-4.
22. Bishop JA, Lewis Jr JS, Rocco JW, Faquin WC. HPV-related squamous cell carcinoma of the head and neck: an update on testing in routine pathology practice. Sem Diagn Pathol. 2015;32(5):344-51. https://pubmed.ncbi.nlm.nih.gov/25724476. https://doi.org/10.1053/j.semdp.2015.02.013.
23. Stevens TM, Bishop J, HPV-related carcinomas of the head and neck: morphologic features, variants, and practical considerations for the surgical pathologist. Virchows Aech. 2017;471(2):295-307. https://pubmed.ncbi.nlm.nih.gov/28417200. https://doi.org/10.1007/s00428-017-2118-y.
24. Nopmaneepaisarn T, Tangjaturonrasme N, Rawangban W, Vinayanuwattikun C, Keelawat S, Bychkov A. Low prevalence of p16-positive HPV-related head-neck cancers in Thailand: tertiary referral center experience, BMC Cancer. 2019;19(1):1050. https://pubmed.ncbi.nlm.nih.gov/31694600. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6836494. https://doi.org/10.1186/s12885-019-6266-0.
25. Shelton J, Purgina BM, Cipriani NA, Dupont WD, Plummer D, Lewis Jr JS. p16 immunohistochemistry in oropharyngeal squamous cell carcinoma: a comparison of antibody clones using patient outcomes and high-risk human papillomavirus RNA status. Mod Pathol. 2017;30(9):1194-1203. https://pubmed.ncbi.nlm.nih.gov/28621317. https;//doi.org/10.1038/modpathol.2017.31.
26. Gillison ML. Human papillomavirus-associated head and neck cancer is a distinct epidemiologic, clinical, and molecular entity. Semin Oncol. 2004;31(6):744-54. https://pubmed.ncbi.nlm.nih.gov/15599852. https://doi.org/10.1053/j.seminoncol.2004.09.011.
27. El-Mofty SK. Human papillomavirus-related head and neck squamous cell carcinoma variants. Semin Diagn Pathol. 2015;32(1):23– 31. https://pubmed.ncbi.nlm.nih.gov/25804342. https://doi.org/10.1053/j.semdp.2015.02.022.