The Utility of Immunohistochemistry in Diagnosing Tubulocystic Renal Cell Carcinoma with Papillary Morphology
DOI:
https://doi.org/10.21141/PJP.2022.02Keywords:
renal cell carcinoma, histology, immunohistochemistry, diagnosis, surgical pathologyAbstract
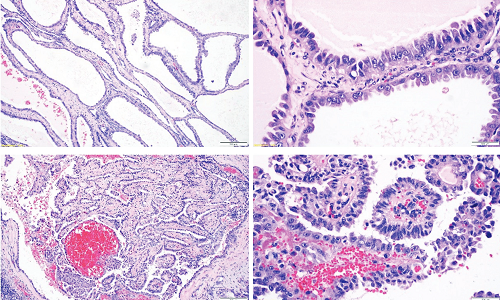
Tubulocystic renal cell carcinoma (TC-RCC) is a recently recognized, rare but distinct malignant entity. Pathologists have endeavored to completely define its histomorphologic, immunohistochemical and molecular features. Recounted is a case where the diagnosis of TC-RCC was confounded by presence of papillary morphology. Immunohistochemical expression of alpha-methyl acyl-CoA-racemase and vimentin with corresponding negativity for CK7 and CD10, following distinctive gross and microscopic findings, confirmed a diagnosis of TC-RCC. This report demonstrates the strategic value of performing immunohistochemistry studies to establish a diagnosis of TC-RCC especially when unusual histologic features are encountered. Immunohistochemistry continues to be the most practical approach to diagnosis as molecular testing methods, such as next generation sequencing, remain unfeasible in the local setting. Cautious prognostication is required as accounts of recurrence and metastasis continue to emerge.
Downloads
References
2. Moch H, Humphrey PA, Ulbright TM, Reuter VE, eds. WHO Classification of Tumours of the Urinary System and Male Genital Organs, 4th ed. Lyon: International Agency for Research on Cancer; 2016.
3. Alfaseh A, Ahmad A, Darraj A, Ilaiwy A. Rare case of tubulocystic RCC in association with papillary RCC. BMJ Case Rep. 2019;12(8): e230191. https://pubmed.ncbi.nlm.nih.gov/31451463. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6720960. https://doi.org/10.1136/bcr-2019-230191.
4. McLennan GT, Cheng L. Neoplasms of the Kidney. In: Bostwick DG, Cheng L, eds. Urologic Surgical Pathology. 3rd edition. Philadelphia: Elsevier; 2020.
5. Truong LD, Shen SS. Immunohistochemical diagnosis of renal neoplasms. Arch Pathol Lab Med. 2011;135(1):92-109. https://pubmed.ncbi.nlm.nih.gov/21204715. https://doi.org/10.5858/2010-0478-RAR.1.
6. Lawrie CH, Armesto M, Fernandez-Mercado M, et al. Noncoding RNA expression and targeted next-generation sequencing distinguish tubulocystic renal cell carcinoma from other renal neoplasms. J Mol Diagn. 2018;20(1):34-45. https://pubmed.ncbi.nlm.nih.gov/29056573. https://doi.org/10.1016/j.jmoldx.2017.09.002.
7. Sarungbam J, Mehra R, Tomlins SA, et al. Tubulocystic renal cell carcinoma: a distinct clinicopathologic entity with a characteristic genomic profile. Mod Pathol. 2019;32(5):701-9. https://pubmed.ncbi.nlm.nih.gov/30622286. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7549436. https://doi.org/10.1038/s41379-018-0185-5.
8. Choi TS, Lee DG, Won KY, Min G. Tubulocystic renal cell carcinoma is not an indolent tumor: a case report of recurrences in the retroperitoneum and contralateral kidney. Medicina (Kaunas). 2021;57(8):851. https://pubmed.ncbi.nlm.nih.gov/34441057. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8398376. https://doi.org/10.3390/medicina57080851
9. Yousuf H, Kumar S, Al-Moundhri M. Rarest of the rare metastatic tubulocystic carcinoma of the kidney. Cureus. 2020;12(12):e12117. https://pubmed.ncbi.nlm.nih.gov/33354487. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7746312. https://doi.org/10.7759/cureus.12117.
10. Salvatori F, Macchini M, Misericordia M, Paci E, Giovagnoni A, Candelari. A simple cyst is not always simply a cyst: a case of cystic recurrence after nephrectomy for tubulocystic renal cell carcinoma and literature review. Urologia. 2020;87(3):119-24. https://pubmed.ncbi.nlm.nih.gov/31441383. https://doi.org/10.1177/0391560319870091.