Pathology, a basic science course in medical schools is a highly visual subject that requires examination of tissues using a microscope. With progressive technological advancements, the use of time-tested optical microscopes in teaching is seemingly slowly replaced by virtual microscopy that many medical schools in developed countries proved its numerous advantages. In our setting, digital pathology is not yet fully integrated in medical school. Although a few medical institutions in the country may have started this technology, there are still a lot to explore with virtual microscopy that will unlock its full potential of revolutionizing medical education in the future.
Key words: digital pathology, virtual microscopy, medical education, pathology education
Pathology is the medical discipline that provides a scientific foundation for medical practice. It is a required basic science course in medical school, and is often the first introduction to human disease processes.[1] Compared with other basic sciences, pathology is a visual subject that is based in part on histopathologic examination of tissues which is important to understanding basic mechanisms of disease processes.
The microscope has been the most widely used instrument in pathology education and until now, is still a mainstay in the classrooms and laboratories of pathologists. However, pathology is under a digital revolution enabled by virtual microscopy – the practice of converting glass microscope slides to high-resolution, whole-slide digital images[2] that some recent studies have demonstrated a decrease in the use of traditional microscopes in medical schools, mainly as a result of current developments in the curriculum as well as some disadvantages of the technique itself.[3]
Whole slide imaging (WSI), also known as digital pathology or virtual pathology, is a technology that involves high-speed, high-resolution digital acquisition of images representing entire stained tissue sections from glass slides in a format that allows them to be viewed by a pathologist on a computer monitor, where the image – often referred to as the ‘whole slide image’ or digitized slide’ can be magnified and navigated spatially in much the same way as standard microscopy.[4] In addition, the digital slide images can be viewed across a network, including the Internet, using specialized viewing software[2] – a potential area for accurate and timely diagnosis in actual pathology practice compared with traditional methods.
Significant technological advancements of digitizing slides and the development of workflow tools that facilitate remote viewing and analysis are likewise enabling pathologists to substantially change how they learn and practice their profession.[2] With the emergence of digital pathology over the past several years, there is an opportunity to revolutionize the way teaching and learning are done in medical schools in the country and would create opportunities beyond classroom teaching.
Trends in Implementation
Digital pathology has already been implemented in many medical schools in the United States and other developed countries and has been shown to provide advantages compared with the usual traditional method of teaching histology and pathology courses.[5],[6],[7],[8] A few of developing countries has utilized the digital pathology in the form of telepathology in clinical practice.[9],[10] Telepathology is the electronic multimedia communication across a network of pathology-related information, between 2 or more locations for use – cases between pathologists and/or qualified laboratory personnel, and may include involvement by clinicians and/or patients.[11] Several journals reported the use of digital pathology in the form of telepathology in education,[12] second-opinion consultations,[13],[14] and primary diagnosis.[15],[16],[17] Success in the implementation of virtual microscopy has been documented in graduate education in medical,[18],[19],[20] dental[21] and veterinary schools.[22] In addition, the US Food and Drug Administration approval of whole slide imaging (Philips IntelliSite Pathology Solution) for primary diagnosis in surgical pathology in 2017 marked a significant evolution of digital pathology.[23] If the current trend continues, the implementation of virtual microscopy may eventually make the time-tested microscope a relic in medical education, and possibly in pathology laboratories.
The Learning Environment
The general pathology course in medical education includes different elements, each with different learning goals. In our experience, these elements include lectures, virtual microscopy lessons and small group discussions. The virtual microscopy session involves 1 teacher per 12 students wherein selected microscopy specimens are scrutinized and allowing students to interact actively. The small group discussions include case studies wherein theory from lectures are combined with information from textbooks, microscopy and clinical data (clinical correlation). Proper alignment of these study elements would allow microscopy to be seamlessly integrated in all aspects of the course, improving microscopy knowledge and performance of the students. From this pioneering experience, we utilized digital pathology in classroom teaching that favors student-centered, self-directed learning. This new framework based on platforms familiar with twenty-first century students will change how they learn pathology – a transition from seeing actual gross and microscopic specimens to looking at images from Web-based resources.
Practical Benefits Over Conventional Microscopy
There are many advantages to using digital pathology or virtual microscopy than with traditional microscope glass slides (Table 1). Digital images can be standardized, with the potential for image enhancement, so that all students will study the exact same tissue section. Microscopic sections on glass slides show variability with regards to quality and content[24] which may often be incomplete and not identical leading to discrepancies in testing and scores of students. These variabilities can be substantially eliminated with digital imaging. Compared to glass slides that are prone to fading, breaking and loss over time, the quality of the image can also be indefinitely maintained with digital pathology.[25] In addition, rare cases of glass slides cannot be duplicated and made available for the students.
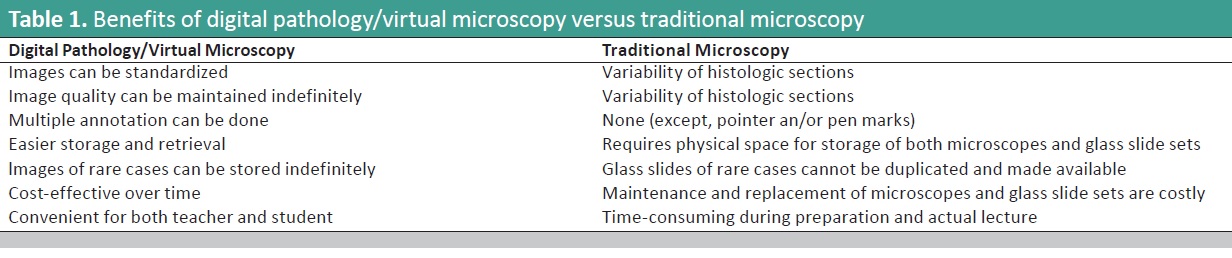
Table 1. Benefits of digital pathology/virtual microscopy versus traditional microscopy
Another very helpful aspect of virtual microscopy is that digital images of microscopic glass slides on a computer screen have panning and zooming capabilities simulating moving the stage and the low to high power magnification of an optical microscope.26 The digital image has a thumbnail image from which the students can always refer to when viewing the digital slides at a higher magnification for proper orientation of histologic sections (Figure 1).[3]
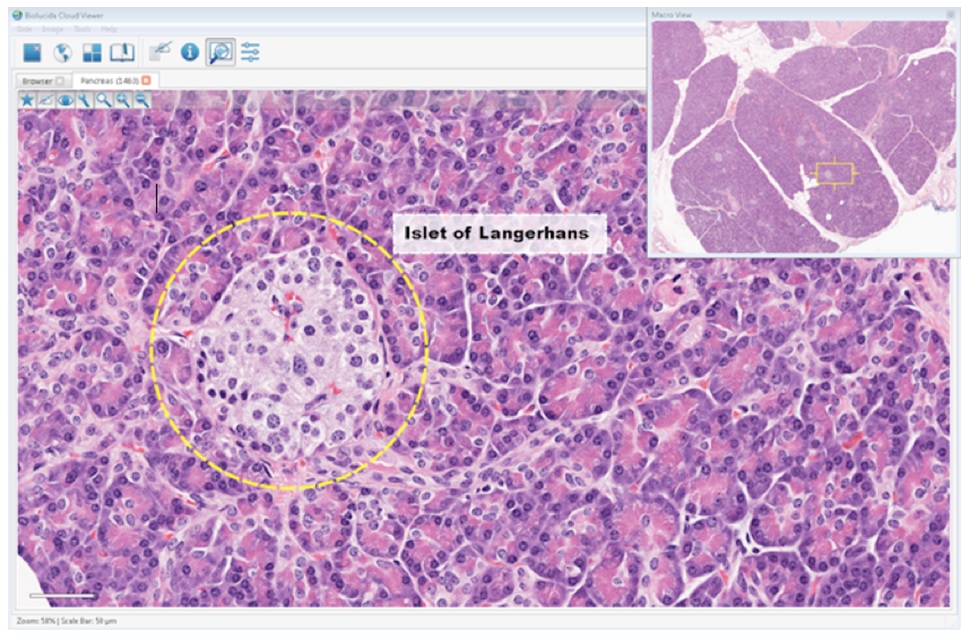
Figure 1. Virtual Microscopy Platform. Screenshot of the digital slide viewer in the virtual microscopy platform showing the pancreas [Online image](2018). Retrieved from https://www.mbfbioscience.com/iowavirtualslidebox.
Conventional microscope glass slides cannot be easily annotated with any precision, and rely on crude techniques like pen-marking/“dotting” (Figure 2) and utilizing eyepiece with pointer for highlighting a certain area in the field (Figure 3). Multiple annotations (arrows, circles, texts, etc.) can be placed exactly where needed in the digital images.[19]
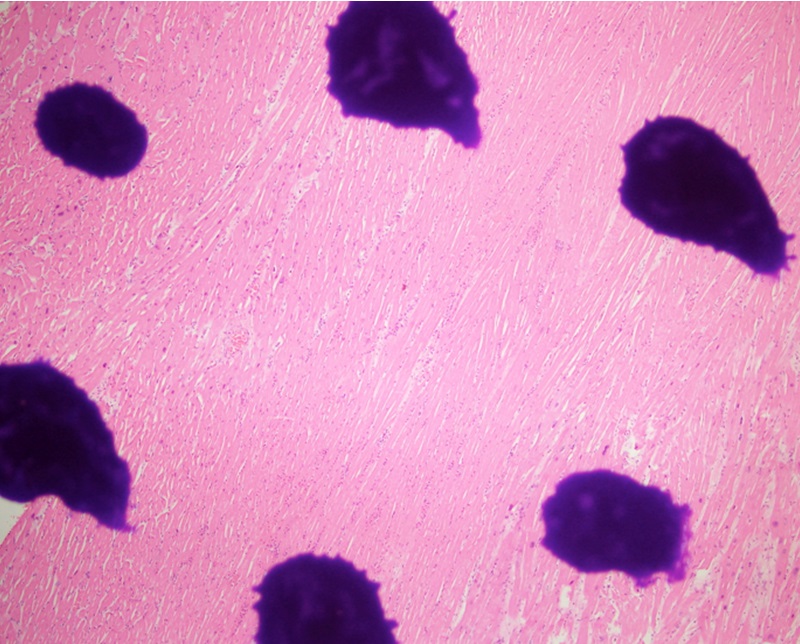
Figure 2. Crude technique of pen-marking or “dotting” on a microscope glass slide. This is a photomicrograph showing the “dotted” area which highlights an acute myocardial infarction (H&E, 40X).
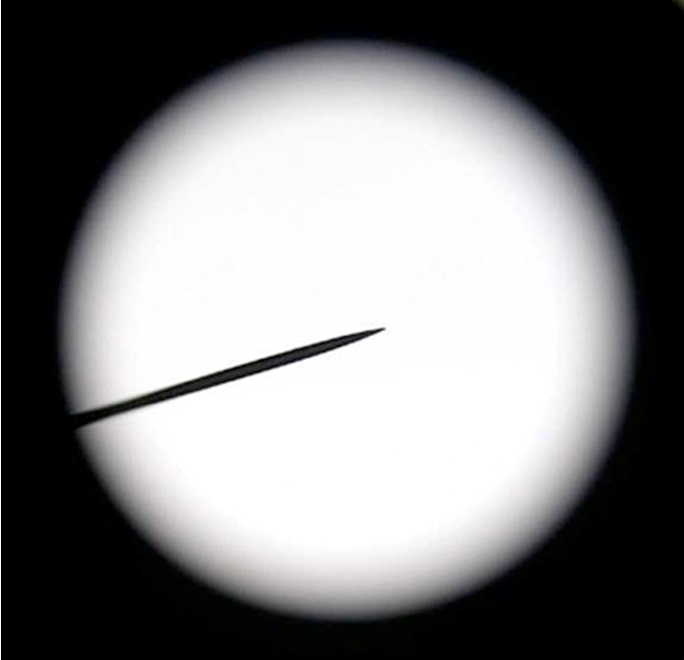
Figure 3. Microscope eyepiece with pointer. This technique is more common in the traditional microscopy classroom to point structure of interest [Online image] (2018). Retrieved from https://www.amscope.com/wf10x-microscope-eyepiece-with-pointer-23mm.html.
Aside from these benefits, the time used for setting up the educational sessions and actual teaching process are much less compared to traditional microscopy, hence giving students more time to learn. The use of the microscopes is often limited to the working hours of the faculty, requiring the students to be physically at school for self review.[19]
With digital pathology where whole-slide images are loaded onto a web-based server, study can occur wherever and whenever the student wishes.[25] Finally, storage and maintenance of microscopes and glass slides sets are cumbersome and require significant expenses.[2] Digital images can be easily stored in server memory or computer disks which provides smooth retrieval.
Impact on Student Learning
The possibility of providing students with all the information they need electronically has been an idealized concept for many years.[27] Web-based resources including social media have shown benefits to supplement education in a cost-effective way. This was certainly one of the reasons for the positive attitude of the students toward digital pathology. Several studies have proven that the majority of students believe that the use of digital slides enhanced their ability to learn.[24],[28]
Virtual microscopy has not only been reported to improve the student learning process, but it has also been shown to improve their cooperation skills, communication abilities and self-confidence.[29] However, some students still find it important for them to be proficient in using the traditional method of viewing the glass slides. The sense of fulfillment of manually operating the microscope – focusing the image, navigating the slides and changing objectives – cannot be satisfied by digital slides. In our setting, the extent of what digital pathology can offer for student learning has yet to be explored which includes remotely reviewing the digital images anytime, anywhere.
Impact on Teaching
The transition from conventional to virtual microscopy presents certain challenges for teachers. The methods of preparing and delivering the lessons changed. Teachers could now prepare lessons at home on a personal computer without requiring access to a microscope.
In addition, there will no longer be any time-consuming, hands-on microscope work during lessons which could create more time for reviewing specimens with the students.[27] Digital pathology has enabled each teacher or course director to customize a collection of scanned slide specimens to suit particular needs. Teachers regarded this flexibility as a positive aspect of virtual microscopy.[27]
Challenges in Implementation
Implementing digital microscopy in medical education may not pose crucial challenges as in diagnostic practice. Unlike in medical education, digital microscopy in the actual practice of pathology requires several important considerations, of which quality slides that are cut and stained properly are a crucial step.
Aside from these, barcode labelling of slides for accurate identification of data entry into database, slide scanning, integration of the scanned data and image-viewing applications into the laboratory and hospital’s information system and the technological infrastructure enabling image transfers must be taken into account.[26]
Digital slides used in teaching are customized according to the topic of discussion. These may not necessarily come from the original scanned glass slides from the Histopathology Section, but may be retrieved from image-viewing applications or pre-loaded digital images by the system provider.
Establishing a digital microscopy laboratory is initially an expensive project, but may eventually become economical than traditional microscopy which relates to additional costs in the storage and maintenance of microscopes and glass slides sets. Dee et al., calculated the cost of a microscope laboratory for 50 students to be about $100,000 per year, which approaches the complete start-up costs for virtual microscopy, including purchase of a virtual slide scanner.[30]
In low resource areas such as in our setting, the challenges are more apparent. Access to the Internet on academic networks is often slow and expensive. Aside from the cost, other barriers include the limited student access to computer workstations especially after class hours, technical aspects such as unreliable electrical power and adverse weather events which could disrupt telecommunications.[31]
Teacher-student interaction is also a concern. It would seem like virtual microscopy would decrease the dynamic interaction between teachers and students. However, in truth, this technology enabled the students to learn pathology in a more interactive and stimulating manner.
Opportunities for Digital Pathology in Education
Although the classroom offers a high utility environment for digital pathology in medical education, many other education-related areas also benefit from the use of digital pathology, including decision support, digital slide conferences, proficiency testing and quality assurance.[2] The possibility of creating a repository of digital slides by pathologists over time can be helpful in decision support.[2]
The accessibility of digital pathology makes it easier to present in seminars, symposia and conferences. Of these scientific presentations, clinicopathologic conference, tumor boards and morbidity/mortality/autopsy audits are among the most commonly encountered meetings by a medical student. Digital slide conferences conducted via the Internet allow multiple participants to view the digital slides simultaneously, and in real-time.[2]
Digital pathology can be utilized in training and education in the form of proficiency testing in other fields of anatomic pathology. It has been shown that proficiency testing in gynecologic cytopathology (“virtual Pap tests”) is feasible.[32] Similar with proficiency testing, the cost and difficulty of glass slides logistics in quality assurance (QA) practices is one of the drawbacks of traditional microscopy. With digital pathology, it is simple to make digital slides accessible to other facilities and organizations for QA programs.[2]
Finally, digital pathology can be utilized in other learning courses such as microbiology, hematology, histology, cytology and clinical microscopy (urine and body fluids) and integrated in online platforms showing educational videos and slide navigation of particular topics in medicine.
Digital pathology is a powerful educational tool that could effectively replace the traditional standard methods of teaching and learning pathology. It provides mobility and convenience to medical students and teachers alike. While majority of the medical schools in the country still consider microscopes and glass slides inevitable in pathology education, we believe that in the coming years, digital pathology will be eventually integrated not only in pathology and histology curricula, but also in other courses requiring microscopy. It will potentially revolutionize medical education and create several opportunities beyond classroom teaching.
All authors certified fulfillment of ICMJE authorship criteria.
The authors declared no conflict of interest.
None.
[1] Naw ME, Thu ZH, San SO. Student’s perception on effectiveness of pathology teaching in phase 1 medical program at UCSI university. IJMSE. 2016;3(3):264-73. http://www.ijmse.com/uploads/1/4/0/3/14032141/ijmse_vol_3_issue__3_page_264-273.pdf
[2] Soenksen D. Digital pathology: a new frontier in education. LabMedicine. 2008;39(2):73-7.
[3] Dee FR. Virtual microscopy in pathology education. Hum Pathol. 2009;40(8):1112-21. PubMed CrossRef
[4] Pantanowitz L, Sinard JH, Henricks WH, et al. Validating whole slide imaging for diagnostic purposes in pathology: Guideline from the College of American Pathologists Pathology and Laboratory Quality Center. Arch Pathol Lab Med. 2013;137(12):1710–22. PubMed CrossRef
[5] Dee FR, Heidger P. Virtual slides for teaching histology and pathology in: Virtual microscopy and virtual slides in teaching, diagnosis, and research. Florida: Taylor & Francis Group, CRC Press, Boca Raton, 2005.
[6] Paulsen FP, Eichhorn M, Bräuer L. Virtual microscopy – the future of teaching histology in the medical curriculum? Ann Anat. 2010;192(6):378–82. PubMed CrossRef
[7] Bloodgood RA, Ogilvie RW. Trends in histology laboratory teaching in United States medical schools. Anat Rec B New Anat.2006;289(5):169-75. PubMed CrossRef
[8] Krippendorf BB, Lough J. Complete and rapid switch from light microscopy to virtual microscopy for teaching medical histology. Anat Rec B New Anat. 2005;285(1):19–25. PubMed CrossRef
[9] Brauchli K, Jagilly R, Oberli H, et al. Telepathology on the Solomon Islands – two years’ experience with a hybrid web- and email-based telepathology system. J Telemed Telecare 2004;10(Suppl 1):14-7. CrossRef
[10] Pagni F, Bono F, Di Bella C, Faravelli A, Cappellini A. Virtual surgical pathology in underdeveloped countries: the Zambia project. Arch Pathol Lab Med. 2011;135(2):215-9. PubMed CrossRef
[11] Pantanowitz L, Dickinson K, Evans AJ, et al. American Telemedicine Association clinical guidelines for telepathology. J Pathol Inform. 2014;5(1):39. PubMed PubMed Central CrossRef
[12] Weinstein RS. The education of professionals. Hum Pathol. 2003;34(5):415-6. PubMed
[13] Molnar B, Berczi L, Diczhazy C, et al. Digital slide and virtual microscopy based routine and telepathology evaluation of routine gastrointestinal biopsy specimens. J Clin Pathol. 2003;56(6):433-8. PubMed PubMed Central
[14] Okada DH, Binder SW, Felten CL, Strauss JS, Marchevsky AM. “Virtual microscopy” and the internet as telepathology consultation tools: diagnostic accuracy in evaluating melanocytic skin lesions. Am J Dermatopathol.1999;21(6):525-31. PubMed
[15] Evans AJ, Chetty R, Clarke BA, et al. Primary frozen section diagnosis by robotic microscopy and virtual slide telepathology: the University Health Network experience. Hum Pathol. 2009;40(8):1070-81. PubMed CrossRef
[16] Dunn BE, Choi H, Recla DL, Kerr SE, Wagenman BL. Robotic surgical telepathology between the Iron Mountain and Milwaukee Department of Veterans Affairs Medical Centers: a 12-year experience. Hum Pathol. 2009;40(8):1092–9. PubMed CrossRef
[17] Tsuchihashi Y, Takamatsu T, Hashimoto Y, Takashima T, Nakano K, Fujita S. Use of virtual slide system for quick frozen intra-operative telepathology diagnosis in Kyoto, Japan. Diagn Pathol. 2008;3(Suppl 1):S6. PubMed PubMed Central CrossRef
[18] Blake CA, Lavoie HA, Millette CF. Teaching medical histology at the University of South Carolina School of Medicine: transition to virtual slides and virtual microscopes. Anat Rec B New Anat. 2003;275(1):196-206. PubMed CrossRef
[19] Foster K. Medical education in the digital age: digital whole slide imaging as an e-learning tool. J Pathol Inform. 2010;1:14. PubMed PubMed Central CrossRef
[20] Boutonnat J, Paulin C, Faure C, Colle PE, Ronot X, Seigneurin D. A pilot study in two French medical schools for teaching histology using virtual microscopy. Morphologie. 2006; 90(288):21-5. PubMed
[21] Chen YK, Hsue SS, Lin DC, et al. An application of virtual microscopy in the teaching of an oral and maxillofacial pathology laboratory course. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105(3):342-7. PubMed CrossRef,/
[22] Mills PC, Bradley AP, Woodall PF, Wildermoth M. Teaching histology to first-year veterinary science students using virtual microscopy and traditional microscopy: a comparison of student responses. J Vet Med Educ. 2007;34(2):177-82. PubMed
[23] Evans AJ, Bauer TW, Bui MM, et al. US Food and Drug Administration approval of whole slide imaging for primary diagnosis: A key milestone is reached and new questions are raised. Arch Pathol Lab Med. 2018; 142(11):1383–7. PubMed CrossRef
[24] Kumar RK, Velan GM, Korell SO, Kandara M, Dee FR, Wakefield D. Virtual microscopy for learning and assessment in pathology. J Pathol. 2004(5);204:611-8. PubMed CrossRef
[25] Goldberg HR, Dintzis R. The positive impact of team-based virtual microscopy on student learning in physiology and histology. Adv Physiol Educ. 2007;31(3):261-5. PubMed CrossRef
[26] Jara-Lazaro RA, Thamboo TP, Teh M, Tan PH. Digital pathology: exploring its applications in diagnostic surgical pathology practice. Pathology. 2010;42(6):512-8. PubMed CrossRef
[27] Vainer B, Mortensen NW, Poulsen SS, et al. Turning microscopy in the medical curriculum digital: Experiences from the faculty of health and medical sciences at University of Copenhagen. J Pathol Inform. 2017;8:11. CrossRef
[28] Hiedger PM Jr., Dee F, Consoer D, Leaven T., Duncan J, Kreiter C. An integrated approach to teaching and testing in histology with real and virtual imaging. Anat Rec. 2002;269(2):107-12. PubMed CrossRef
[29] Weinsten RS. Innovations in medical imaging and virtual microscopy. Hum Pathol. 2005;36(4):317-9. PubMed CrosRef
[30] Dee FR, Meyerholz DK. Teaching medical pathology in the twenty-first century: virtual microscopy applications. J Vet Med Educ. 2007;34(4):431-6. PubMed CrossRef
[31] Fontelo P, Faustorilla J, Gavino A, Marcelo A. Digital pathology –implementation challenges in low-resource countries. Anal Cell Pathol. 2012;35(1):31-6. PubMed PubMed Central CrossRef
[32]Marchevsky AM, Khurana R, Thomas P, Scharre K, Farias P, Bose S. The use of virtual microscopy for proficiency testing in gynecologic cytopathology: a feasibility study using Scan Scope. Arch Pathol Lab Med. 2006;130(3):349-55. PubMed CrossRef